Bridging worlds
Inaugural OUWB alumni and current student event tackles the questions on the minds of future physicians
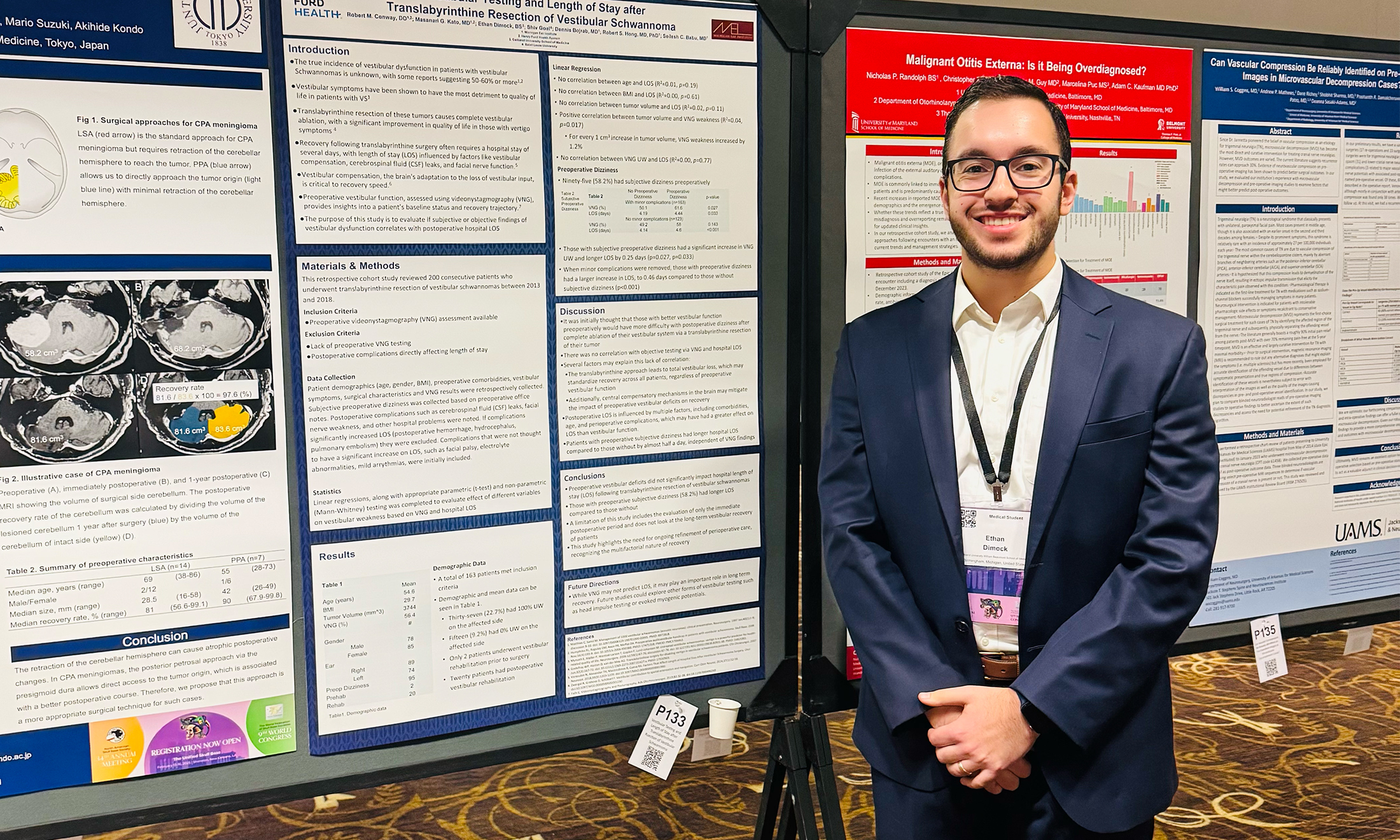
The Inaugural Alumni and Student Networking Mixer and Panel Discussion at OUWB recently saw a handful of alumni from the school sharing their valuable experiences and insights with current students.
The event was held this past spring at Corewell Health William Beaumont University Hospital in Royal Oak.
Participating alumni were Chris Jaeger, M.D., OUWB ’15 (urology); Yujin Oh, M.D., OUWB ’18 (family medicine); Nate Loudon, M.D., OUWB ’20 (interventional radiology); Melissa Bayci, M.D., OUWB ’15 (OB-Gyn); and Alison Thomas, M.D., OUWB ’20 (OB-Gyn).
Together, they touched on various topics: choosing and pursuing a specialty; general practical tips on navigating medical school and residency; and what they wish they had done differently.
“We’re really excited to be able to bridge these worlds of students and alumni,” said Berkley Browne, Ph.D., associate dean, Student Affairs. “We’ve been working pretty aggressively on developing some more programming like this so this is just the start.”
The alumni fielded questions and addressed topics based on submissions from attendees received prior to the event. Here is an annotated version of the questions and responses.
Q: How did you pick your specialty? How did you narrow it down for all the choices?
Thomas: I thought a lot about options during M1 and M2 years, but none of that was relevant until I started rotations in my third year. Just keep an open mind. I did not plan my life around OB at all, but from day one I was just amazed…very excited and happy.
Bayci: I knew I wanted to do OB for a while. I am passionate about women’s health and being able to be there for women through all different aspects of their lives, whether they’re teenagers, or trying to get pregnant, or pregnant, all the way into menopause. It’s nice to be that person for those people during vulnerable times of their life.
Loudon: I didn’t want to get locked into (treating) one organ system or one part of the body. I wanted to think about and treat diseases across as many different organ systems as I could. And I really like procedures. All of that together led me to IR (interventional radiology) and diagnostic radiology.
Oh: From early on, I just always liked the idea of being a jack-of-all-trades…rather than being a specialist. During medical school, going through rotations, I found myself pretty much enjoying everything…so I decided to stick with it.
Jaeger: I got into medicine in large part because of a urologist. But I just wanted patients to do better…that’s naturally where urology comes into play. Our patients generally leave either the same day as surgery or the next day, and they’re very grateful you did something to help their quality of life.
Q: What does a typical day look like, and has your specialty choice met your expectations?
Jaeger: It’s either in the operating room or the clinic. As a pediatric urologist, we see a lot of kids in the clinic and thankfully we don’t need to operate on the vast majority of them. But the ones we do operate on need fairly complex things at times. It has definitely met my expectations. It’s hard to find more rewarding things in medicine than a kid getting better for something that you did.
Oh: I’m doing all outpatient medicine right now. Obviously, lifestyle was a big factor in making that decision. In terms of meeting expectations…a big part of why I wanted to do family medicine was being able to build long-term relationships with patients. Although I’m not too far into my practice, I’m seeing same family members, their relatives and friends…those are the most gratifying moments for me.
Loudon: It has met my expectations. As far as day-to-day, it’s a two-part answer. On diagnostic days, my typical workday is 8 a.m. to 5 p.m. On the IR side, days tend to start a little earlier…you round on your patients and do procedures. You’ll be going home around 5 p.m., and potentially later if you’re on call.
Bayci: (As an attending) I’m usually in the office three days a week, seeing a mixture of annuals and doing procedures…and follow-ups. I’m on call once a week and it’s a 24-hour call. Sometimes you’re there for 24 out of the 24 hours, while other times you go in and round and don’t have much else going on. The hours can be long, but I enjoy what I do…there have been times when I’m leaving the hospital at 2 a.m. and I just did a great delivery and I’m really happy that I was able to be there and do that for that person.
Thomas: A day in the life of an OB resident is unique. We rotate in the subspecialties. We have a morning huddle at around 6:45 a.m. and I’m usually here until 5:30 p.m. As a fourth year, we do 24-hour shifts every sixth day and then I’m off the next day, which is nice. It has definitely met my expectation…the highs are really high and they’re more common. I’m grateful that I chose this specialty.
Q: What do you wish you had known or done differently as an M1, M2, or even an M3 student to set you up for success and make the transition to residency a little bit easier?
Thomas: I think trusting the process more. There’s a reason for the things that you’re doing and it’s going to be OK. If medical school is like drinking out of a fire house, residency is 10 times worse. But it’s great, and you’ll be fine.
Bayci: Two things. First, make sure you remember who you are as a person. I think a lot of the times as medical students, that can be your entire identity and then in residency, that becomes your entire identity. When I got to attending life, I was like “What am I other than what we’re doing? I have no idea.” So, I’m kind of reinventing myself. The second thing is to not get ahead of yourself. M1s and M2s…please don’t start thinking about match. Don’t start thinking about tracks. Think about your next exam. You should be worried about doing well in your classes. Don’t let yourself spiral and stress out about things that are way in your future.
Loudon: Med school will fill whatever amount of space you give it. That means it can take over your whole life. Or you can put it in this little box and pretend like it doesn’t exist and struggle. You’ve got to find the balance. I would not be as stressed as I was and so neurotic about not only studying, but this life identity crisis…because you’ve got three or four short years to figure out basically your whole future. It’s fine. Don’t worry about it. Do put in the work, do your thing, but realize you’re going to get through it.
Jaeger: From a more practical scenario, I would say to take (objective structured clinical examinations) like breaking bad news more seriously. It may seem like just another OSCE…but when you’re a first- or second-year resident and you have to break bad news in the middle of the night and there’s not a faculty member in sight or senior resident to help you, you’ll wish you remembered some of those pearls a bit more.
Oh: One, take care of yourself. Take care of your physical and mental health. This is something that’s going to pay off when you go into rotations because it can be really physically demanding. Second, try to have an open mind and enjoy everything. Some of the stuff that you’ll do in clinical rotations will be the last time you do it, but it’s really cool stuff most people in the world don’t get to experience so just try to soak in everything and have fun.

 August 07, 2024
August 07, 2024
 By Andrew Dietderich
By Andrew Dietderich