‘A better researcher’
Six OUWB students participate in two-month program dedicated to diabetes research
Six OUWB medical students spent the summer in a research program sponsored by the National Institutes of Health through the National Institute of Diabetes and Digestive and Kidney Diseases.
The Medical Student Research Program in Diabetes allows medical students to conduct research under the direction of established scientists in the areas of diabetes, hormone action, physiology, islet cell biology, and/or obesity.
Research is conducted at one of 16 National Institute of Diabetes and Digestive and Kidney Disease (NIDDK)-designated diabetes research centers in the U.S., affiliated with such institutions as Stanford University, University of Washington, and Vanderbilt University Medical Center.
The program aims to help students gain an improved understanding of career opportunities in biomedical research and a comprehensive understanding of diabetes, its clinical manifestations, and its unsolved problems. Research projects are presented at an end-of-program conference held in Nashville.
Participants from OUWB in 2022 were M2s Emily Babcock (Vanderbilt), Fanny Huang (Stanford), Nikki Nguyen (Washington), Nikita Patel (University of Colorado), Aubriana Perez (Vanderbilt), and Matthew Prevost (University of Chicago).
“The opportunity to participate in this program has offered me valuable insights into clinic work and translational research of a physician,” said Huang.
Others shared similar thoughts.
“This experience helped solidify my interest in pursuing a career in academic medicine,” said Perez. “It was invaluable being able to learn from some of the most brilliant physician-scientists in their field.”
“My first — and bigger — takeaway was that I got to see how interdisciplinary a common health condition like diabetes is,” said Nguyen. “My second big takeaway from the experience was learning how to troubleshoot and be open-minded.”
‘A better researcher’
According to statistics from the Centers for Disease Control and Prevention (CDC), 37.3 million Americans — about one in 10 — have diabetes. An estimated 96 million American adults — more than one in three — have prediabetes, or a health condition that increases a person’s risk of Type 2 diabetes and other chronic diseases. Without major interventions, the CDC predicts that as many as one in three adults in the United States could have diabetes by 2050.
OUWB students who dedicated their summer to the Medical Student Research Program in Diabetes said they took a lot away from the experience.
Perez, for example, said she grew up in Guam, and noted that many Asian Americans and Pacific Islanders “experience a disproportionately high burden of chronic diseases, such as diabetes and end-stage kidney disease.”
“Naturally, my research interests gravitated towards these areas of medicine,” she said.
| More from OUWB |
|
Study: OUWB among top feeder medical schools for urology Study led by OUWB students finds TikTok medical videos can be improved |
Perez spent the summer at the Vanderbilt University Medical Center’s diabetes research center. She was involved in a number of research activities, ranging from literature reviews of health literacy in chronic kidney disease, to scheduling research visits and performing primary data collection, to cleaning data and performing statistical analyses.
“In graduate school, I was involved in a number of projects focused on addressing social determinants of health in patients with kidney disease, and I felt that I wanted to continue expanding my research experience in this area,” she said. “I specifically applied to the program at Vanderbilt because of their nephrology concentration.
Prevost said he was looking for an opportunity that allowed him to “get a different experience, in a different place and environment, at a different university…not only to represent my school, but to experience something new.”
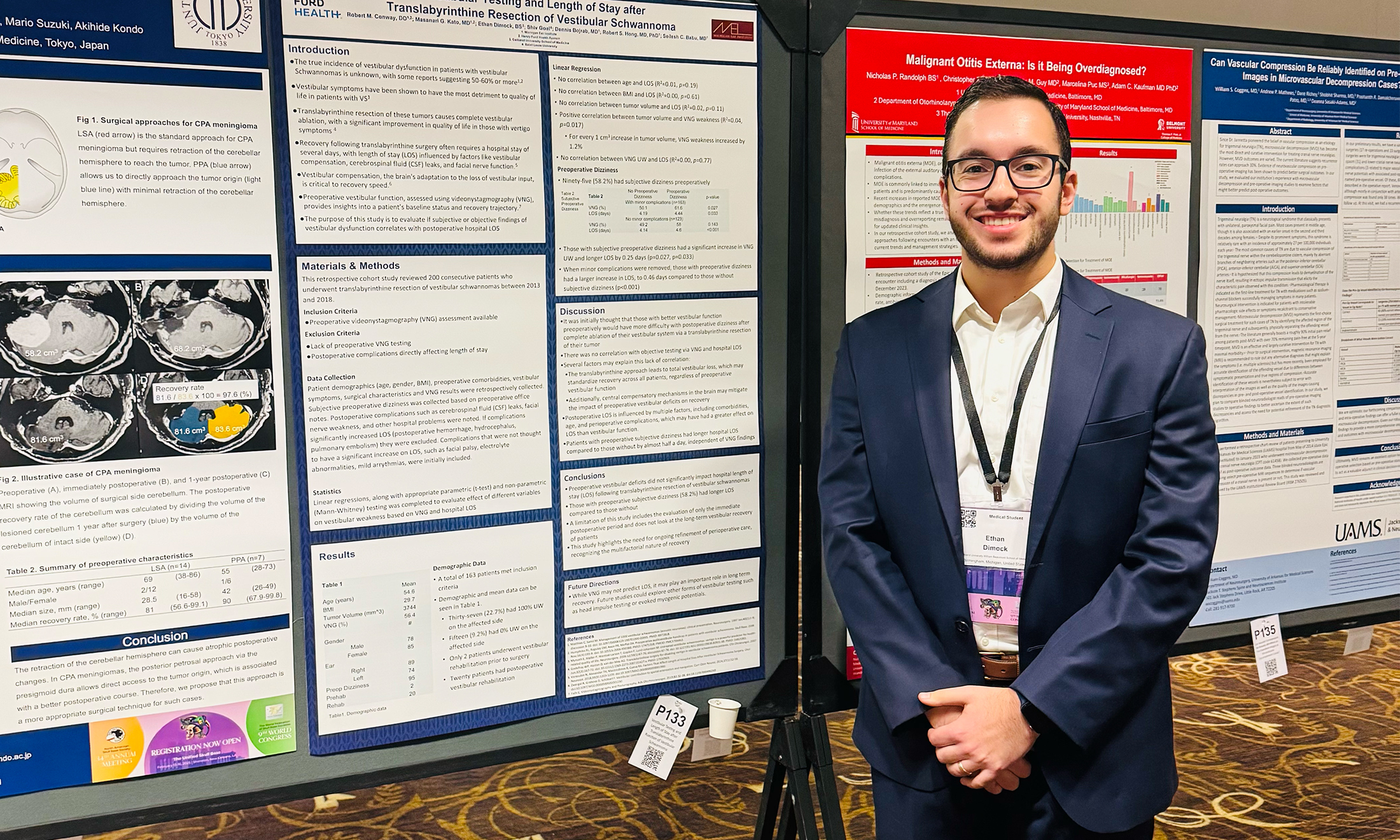
He spent the summer at the University of Chicago, where he led a project called “Three-Dimensional Analysis of Pancreatic Islet Capillary Density: Interspecies Comparison.”
“I learned a lot about diabetes and I think that was the thing…teaching yourself about the topic, learning how to research with others, and how to effectively present and display this information,” he said.
Nguyen said she also wanted to learn more about research, particularly in the areas of gastroenterology, endocrinology, and nephrology. She spent the summer at the UW Diabetes Research Center at South Lake Union in Seattle.
She worked with a doctor who studies complications of diabetes and in particular the mechanisms around atherosclerosis and the role of the apolipoproteins.
“I feel that the NIDDK experience made me both a better researcher and clinician,” she said. “It gave me more appreciation for those who start the research in basic sciences/at the ground up, reminded me of some of the overall limitations in some of the studies we do, and reminded me the importance of understanding the pathophysiology in determining diagnosis and management.”
Huang spent her time in the program at Stanford University. Her project was a longitudinal study on clinical and ophthalmic imaging biomarkers that may predict worsening vision in patients with diabetic retinopathy that Huang designed with the help of her research mentor.
Huang was able to complete an entire project (including data collection and data analysis on over 300 patients over 5 years of clinical care) and curate a poster for the end-of-program research conference.
She said she sought a way to maximize the summer break between M1 and M2 and was pleased to find the NIDDK program because it “aligned well with my personal interests in nutrition and endocrinology-related translational research and allowed me to conduct research at well-renowned diabetes centers across the nation.”
“My primary takeaways from this experience are that it takes a lot of time and teamwork (especially from biostatisticians) to complete a research project, but it is possible with a talented team, and research inspires curiosity as there are infinite unanswered questions out there that researchers can explore,” she said.
Huang encouraged other medical students to consider the program.
“I highly encourage M1s to apply to this program, even if you are not interested in diabetes, endocrinology, gastroenterology, nutrition-related work as a physician,” she said. “These are interdisciplinary areas that can be matched with any specialty, such as my experience with researching diabetes and how that relates to ophthalmic care, and this was a structured program designed to integrate innovative research projects into eight weeks for medical students.”

 December 21, 2022
December 21, 2022
 By Andrew Dietderich
By Andrew Dietderich