OU-Beaumont research could translate to improved cancer treatment
In collaboration with researchers from Oakland University and Beaumont Research Institute, recent Ph.D. graduate Tyler Parsons found that tumors use blood stem cells to evade radiation therapy
A research study conducted by Oakland University and Beaumont Research Institute is providing new insights that could lead to more effective treatment in lung cancer patients.
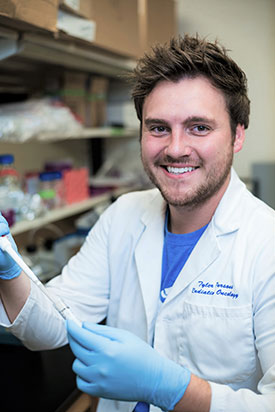
Dr. Tyler M. Parsons worked with researchers from Oakland University and Beaumont Research Institute on a study showing how tumors hijack blood stem cells to evade radiation treatment.
Published in the British Journal of Cancer (Nature Publishing Group), the study showed, for the first time, that solid tumors hijack blood stem cells to aid in treatment evasion. This discovery built upon previous research in Dr. Gerard J. Madlambayan’s lab at OU.
“We knew from previous research in Dr. Madlambayan's lab that blood stem cells are called to the tumor after radiation, and we also knew that the presence of these cells correlated with growth and regrowth of tumors, but we didn’t know if there was a causal relationship between the two,” said Dr. Tyler M. Parsons, the study’s lead author and researcher and a recent graduate of OU’s Ph.D. program in biological and biomedical sciences.
“Through this research, we were able to experimentally demonstrate that one of the important roles of these cells is differentiating into a cell type (M2-polarized macrophage) within the tumor, which directly aids in tumor growth and regrowth.”
Once they determined the role of blood stem cells in benefitting tumors, the researchers sought a way to disrupt the cell differentiation process. They succeeded by adding a drug that inhibits macrophage colony stimulating factor-1 (CSF-1) and using hyperfractionated radiation, as opposed to single beam which is current standard of care for most lung cancers.
“CSF-1 is known to drive blood stem and progenitor cells to turn into tumor-benefitting cells,” said Dr. Parsons. “Our research showed that using a drug that inhibits CSF-1 production, along with hyperfractionated radiation treatments, resulted in improved tumor-killing in mice, compared to standard radiation treatments alone.”
Dr. Parsons added that “hyperfractionated radiation delivery was already in clinical trials for a different type of cancer (glioblastoma) at Beaumont “so there was clinical precedent for the choices we made with the radiation dosages.”

Dr. Parsons is pictured with Dr. Gerard J. Madlambayan after graduating with his Ph.D. in Biological and Biomedical Sciences in spring 2021. Dr. Parsons is now a hematology-oncology postdoctoral research fellow in the Division of Oncology at the Washington University School of Medicine in St. Louis.
The research was performed in the labs of Dr. Madlambayan, associate professor of biological sciences at Oakland University, and Dr. George Wilson, chief of radiation biology and scientific director of the BioBank at Beaumont Health System. Both were co-authors on the study, along with Katie L. Buelow and Alaa Hanna, who worked in the radiation oncology department at Beaumont; Ph.D. student Marisa A. Brake, undergraduate student Crystal Poma and faculty members Drs. Sarah E. Hosch, Randal J. Westrick and Luis G. Villa-Diaz, from OU’s Department of Biological Sciences.
“The collaboration between OU and Beaumont was pivotal and allowed us access to resources to complete a study of this capacity,” said Dr. Parsons, who began working on the project as a Ph.D. student. “The research went on to be the bulk of my dissertation.”
The hope is to translate these findings to clinical practice, which could have a wide-reaching impact on health care.
“While our studies focused on non-small cell lung cancer, this therapeutic strategy could easily be applied to a variety of solid tumor types,” concluded Dr. Madlambayan. “Tyler’s persistence and hard work resulted in a novel and significant finding that could benefit those suffering from cancer.”
Dr. Parsons is now a hematology-oncology postdoctoral research fellow in the Division of Oncology at the Washington University School of Medicine in St. Louis.

 February 16, 2022
February 16, 2022