Among the many unique challenges COVID-19 presented Oakland University William Beaumont School of Medicine, one was clear: the need for a swift response to keep medical students on track.
The reason?
Cancelling the remainder of the school year wasn’t an option as many students — particularly third- and fourth-years — are in the homestretch of their respective medical school educations, set to soon join a field very much in need of new doctors.
Instead, Cynthia Ledford, M.D., associate dean for undergraduate clinical education and professor in OUWB’s Department of Foundational Medical Studies, led a team that responded quickly and creatively. Among other things, efforts included rescheduling exams, developing new electives, and “deconstructing clerkships.”
“We had to step back and ask ourselves ‘What is it that you have to do to learn? To enable the student to learn what they must learn?’” said Ledford. “The hard part is we didn’t have any time to figure this out — we’re literally figuring it out overnight.
“The good news is so is everybody else nationally,” she added. “Our national groups have really been open with sharing resources and suggestions and trying different things.”
For first- and second-year students — who spend most of their time in the classroom — it was a relatively smooth transition to online learning that included use of platforms like WebEx and the ability to draw from the school’s significant archive of recorded classes. (More details about those efforts may be found here.)
For third- and fourth-year medical students — who spend more time in a clinical setting with patients — things were more complicated.
“Our students’ time is valuable and we want them to be able to learn optimally to the max that they can,” said Ledford. “We have to continue the education...and take advantage of the time and resources that we have, which is really what we’re doing.”
OUWB third-year student Michael Brennan, a Medical Student Government (MSG) senator, said the process has included input from students via MSG representation.
“There’s a true appreciation for the school and how much they’re trying to keep us on time with these outside-the-box solutions,” he said. “Because the flipside would have been ‘OK everybody, sit at home for four months until we can get back.”
Getting to the finish line
Though medical students were removed from clinical settings in early March, the importance of the last two years of medical school cannot be overstated.
Third-year medical students (M3s) average about 55 hours of work a week as they ramp up learning compared with their first two years of medical school.
“That’s a full-time job plus,” said Ledford. “There is an incredibly steep learning curve during the third year. So even if their third year is disrupted, we can’t have them do nothing until COVID-19 is gone — especially if you think about the fact that COVID 19 is not going to be completely gone for a year or more.”
Concurrently, fourth-year medical students (M4s) were about six weeks from graduation when the pandemic began to affect daily life. Those six weeks typically contain myriad learning experiences necessary prior to becoming doctors.
“We just needed to get them across the finish line,” she said. “But at the same time, we do not want them starting their residencies unprepared.”
Ledford said OUWB “absolutely” had to take steps to make sure the fourth-year students are well-prepared, and that “they have opportunities to practice skills that they will soon be using with real patients.”
Keeping M3s on track
In early March, M3s were in a time of transition.
Neurology, psychiatry, and OB-GYN clerkships were a week or so from wrapping up.
Eight-week clerkships for surgery, pediatrics, and internal medicine had just started.
Whether students were wrapping up or just starting, they were removed from the clinical setting.
On top of it all, Ledford said it’s important for M3s to stay on track because the process of applying for post-graduation residencies begins in June — almost a full year before they are set to graduate in May 2021. They also have to be on track for sub-internships.
Those were just some of the variables Ledford and her team had to consider when jumping into action.
“Students still had time to do all of the non-clinical learning — acquiring the knowledge, practicing some of the basic clinical skills, reviewing how to make a diagnosis, how to interpret tests,” Ledford said.
That’s exactly what they’ve been doing for the past six weeks, she said.
“Everything that we can do remotely is really what we’re looking at...anything we can give students to learn outside of the clinical setting,” she said.
Ledford said students will still get the patient care portions of their clerkships, though they will in a truncated manner. At this time, it still remains to be seen when that might happen.
“The absolute minimum we need is half the time, or four weeks,” she said. “We’re going to have to make sure students can learn twice as well and twice as quickly because they have half the time.”
Ledford said her team is looking closely at the most critical parts of clerkships to make sure they are part of the in-person training.
For example, she said, there are some parts of the OB-GYN clerkship (labor and delivery) that must be learned in the clinical setting.
“Same thing when they go to the operating room...which types of surgeries do students need to see, what are they supposed to learn in that setting?” Ledford said. “It’s really looking at how they can most efficiently and effectively learn what they need to learn within the shortest amount of time.”
Another change for M3s has been the use of objective structured clinical examinations (OSCEs), or tests typically conducted in the clinical setting to measure proficiency. Ledford said those tests have been moved to a virtual setting through the use of platforms like WebEx.
In addition, M3s have been allowed to take some online electives that they might otherwise take in their fourth year.
Helping M4s reach the finish line
M4s were just weeks away from graduation when COVID-19 started changing things.
They will still graduate on time, but the weeks leading up to graduation typically are packed with learning and testing.
As a result of COVID-19, however, several changes were enacted for M4s, including:
- The NBME emergency medicine exam was rescheduled and done via remote proctoring.
- Ten new online electives were created to allow students to make elective changes for April and May.
- A student-centered, multi-modal approach was developed for students considering entering residency early.
- Beaumont physicians developed opportunities for students to voluntarily contribute to the much-needed efforts related to COVID-19, either in remote health care delivery or research (remote and non-remote).
Like the M3s, several important clinical experiences transitioned to a remote setting.
Take the Diagnostic Medicine clerkship, a requirement for M4s.
Before COVID-19, the clerkship was run with multiple small group discussions that included taking unknown cases real-time with radiology/pathology staff members over 10 sessions.
Each day had a common theme and both pathology and radiology taught to the theme with many overlapping cases. The unknown case material was available through Moodle after each session for review. An exam for pathology and radiology was given on the last day.
COVID-19 forced the entire rotation to move to a remote setting, said Rachel VanHulle, M.D., assistant professor, Department of Diagnostic Radiology and Pediatrics, OUWB, and clerkship director, Diagnostic Radiology, Beaumont Children’s Hospital.
Now, the rotation uses a combination of live and recorded Skype sessions and/or material on the learning platform called Moodle.
It’s a system that was put in place over the course of one weekend.
“Basically, I woke up on a Saturday morning and realized we could be in quarantine soon,” VanHulle said, adding that prompted her to begin exploring ways to continue the clerkship remotely. “Thankfully, this was started because on Sunday afternoon I got the news that all students would be learning remotely starting Monday (March 16).”
VanHulle said of the participating students, “99 percent were very adaptive to change.”
“Most realized many factors were out of our control,” she said. “Also, we were prompt to address any concerns. We continually asked for feedback during and after sessions.”
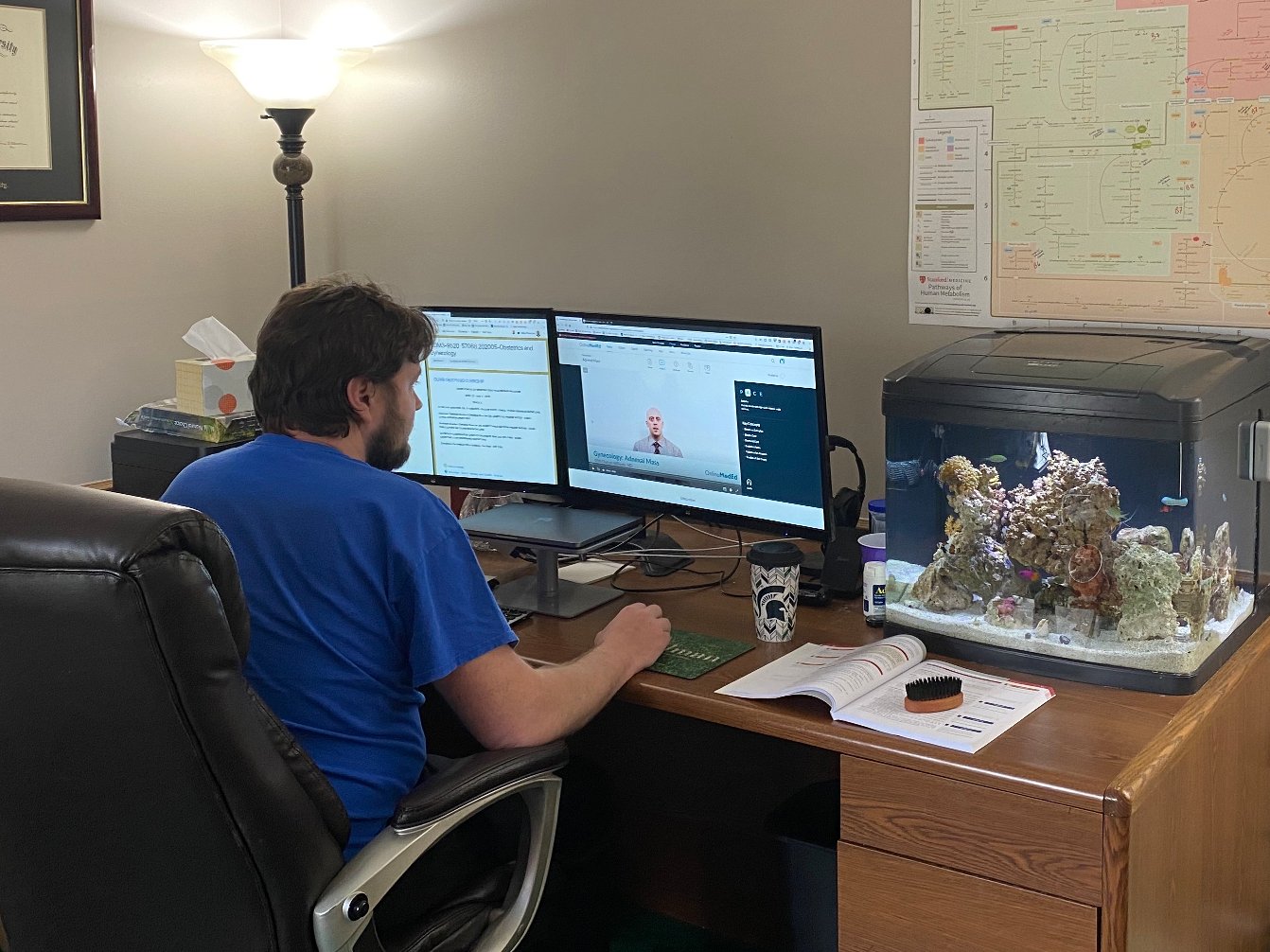
Brennan, who said he is staying on track with his studies at home, said he appreciates how hard school officials have worked to keep students like him on track.
“We’re still working through how many aspects of this can work, but I think it’s an absolutely a blessing that they’re willing to really try to find ways to keep us on track,” he said.
For more information, contact Andrew Dietderich, marketing writer, OUWB, at [email protected].
Follow OUWB on Facebook, Twitter, and Instagram.
NOTICE: Except where otherwise noted, all articles are published under a Creative Commons Attribution 3.0 license. You are free to copy, distribute, adapt, transmit, or make commercial use of this work as long as you attribute Oakland University William Beaumont School of Medicine as the original creator and include a link to this article.

